Uniting One Health and food systems for a more sustainable and inclusive world
Thanks to the COVID-19 pandemic, zoonotic disease epidemics are currently among the most high-profile public health issues. The story of this pandemic cannot be told without reference to food systems, and food markets in particular. But COVID-19 is far from being the only zoonotic disease whose story arises in food systems.
Take Chagas, a disease endemic in 21 Latin American countries and affecting six to seven million people world-wide. Transmitted by the triatomine or kissing bug, it is generally considered a vector-borne disease closely associated with poverty. People become infected by scratching a bite from an infected triatomine bug, which spreads the bug’s fecal matter into the bite wound. But the ecology of Chagas is changing. Starting in the mid-2000’s, a growing number of acute Chagas cases were reported in the Amazon basin, killing dozens and affecting hundreds of people. The outbreaks in the Amazon were notable in part because they were evidence that Chagas had found a new mode of transmission: food. In most of these new cases, people had become infected through eating food contaminated by infected triatomines or their feces rather than through bites.
While a One Health approach can help elucidate the evolving mechanics of the transmission of Chagas disease – from insects, to animals and to fruits, to humans – the full story requires an understanding of food systems. Slash and burn agriculture, a common practice used to open up more land in the Amazon forest for cultivation, created the perfect habitat for the triatomine bug. Concurrently, açai berries grown from certain palms in the area were becoming an increasingly popular commodity in global food markets. These economic pressures from the global food system intersected with human, animal and environmental health to create ideal conditions for the proliferation of acute Chagas.
The story of Chagas illustrates how the threat and spread of zoonoses are best understood by combining a One Health approach with knowledge of food systems. The challenge is that food systems are largely missing in the field of One Health, and vice versa, food systems research could do more to integrate the strengths of a One Health approach.
What’s in a food system, anyway?
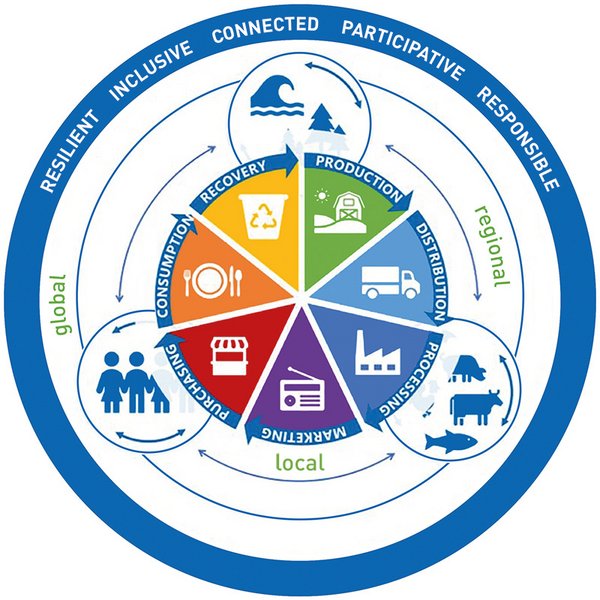
Much like One Health, food systems are characterised by complex interdependencies between multiple actors. This includes all the interlinked actors in the supply and value chains for food products, from the production stage through to processing, packaging, distribution, consumption and waste management. Food systems also include the broader economic, societal and natural environment that supports them.
Sustainable and climate-resilient food systems are a key ingredient of achieving many of the Sustainable Development Goals (SGDs), including zero hunger, good health and wellbeing, responsible consumption and production, climate action, life below water and life on land. Sustainable food systems deliver food security and nutrition for all while ensuring that the production methods of today do not compromise the food security, nutrition and health of future generations. Food systems are considered resilient if they can withstand or rapidly bounce back from major shocks, such as pandemics or extreme weather events resulting from climate change.
Lost ground on SDG 2: No Hunger
After a decade of improvement in the rate of world-wide undernourishment, progress halted and faltered starting in 2014. The prevalence of undernourishment has increased since 2014 and extends to 2019. Today, there are 60 million more undernourished people than there were in 2014. Between 2018 and 2019 alone, the number of undernourished people increased by 10 million.
A long way to go to achieve climate-resilient food systems
There remains considerable work to be done on food systems globally to ensure that they become sufficiently resilient and sustainable. Our food systems remain vulnerable to economic and climate shocks, recurring issues of food insecurity, and their capacity to promote healthy, sustainable and affordable food is decreasing. This has been shown most recently by the COVID-19 pandemic, which could significantly exacerbate the already rising number of hungry people world-wide. This human health and economic crisis bears the risk of halting or undoing progress on the SDGs, many of which are not on track to be achieved by 2030. Meanwhile, we must also contend with climate change, which is deepening global inequalities and affecting food production and availability, in turn affecting nutrition and global health. The links between social and environmental change are contributing to the rise in hunger and problems of access to healthy food.
Reversing these trends will be difficult. We are living in an era in which human and environmental crises are frequently occurring together in what can be described as compounding calamities. These events, many of which are accelerated by climate change, are creating additional stressors on the food system and threaten our ability to produce enough healthy food and make it accessible to all. Mitigating these compounding calamities and making up lost ground on SDGs requires strengthening the resilience of food systems and thinking in more integrated ways to transform food systems for the better. Knowledge and innovation can help build up the equity, diversity and sustainability of food systems and increase their resilience to climate change while also promoting better health, nutrition and resilience to other shocks, pandemics included.
Compounding calamities in East Africa
In 2020, areas of East Africa experienced a rapid-succession series of severe health and environmental crises: COVID-19, devastating floods and the worst infestation of desert locusts in over 25 years. These events each impacted local food systems and compounded one another, increasing the vulnerability of local populations and reducing their ability to engage in social distancing and to practise basic hygiene measures. The same weather conditions that contributed to the locust infestations also affected crop growth and food prices. Food supplies diminished by the locust pest were further diminished by flooding, deepening local food insecurity.
In 2020, East Africa experienced the worst infestation of desert locusts in over 25 years. Photo: Sven Torfinn/ FAO
Knowledge of food systems can enrich One Health, too
The other side of the coin is that food systems research has a lot to offer the One Health approach. High-profile issues that require a One Health approach, namely zoonotic diseases and antimicrobial resistance (AMR), are challenges that arise in food systems and, ultimately, affect them as well. A One Health approach anchored in an understanding of food systems is needed to develop primary prevention methods.
Consider this: an estimated one billion farmers world-wide depend on livestock for their livelihoods, their nutrition and as a form of household insurance. Women who own and are responsible for caring for their household’s livestock face a particular set of challenges due to restrictive gender norms and persistent inequalities. For them, livestock can be an important source of employment and financial security. The livelihoods of these populations are therefore based on living in close proximity to livestock. Depending on the setting, these livestock smallholders or their animals may also be in close contact with local wildlife. These factors put them at increased risk of zoonotic diseases. Since livestock smallholders generally operate in resource-poor settings, measures to reduce disease outbreaks, such as vaccines or cull-and-compensate, are hard to access and implement. Tackling the risk of zoonotic pandemics requires a deep understanding of these interactions as well as the socio-economic and cultural contexts in which they take place.
World-wide, livestock production is also contributing to the emergence of AMR. In the food industry, it is common for antibiotics to be overly used on healthy livestock and fish to promote growth and prevent disease. This is creating environments that hasten the natural process by which microorganisms develop defences to these threats and become resistant to treatment. Alarmingly, the emergence of multi-drug-resistant bacteria, so-called “superbugs”, threatens to usher in a future where the simplest medical procedure can lead to devastating complications as a result of untreatable infections.
The full scope of the problem, especially in low- and middle-income countries, is unclear, and monitoring and tracking systems are lacking. But there is strong evidence that this is a global problem, whose spread into low- and middle-income countries is facilitated by intensive animal production systems that are proliferating to meet the rising global demand for animal protein. Global AMR hotspots have been identified across the Global South, notably in India, China, Pakistan, Iran, Turkey, Brazil, Egypt and Vietnam, and in the areas surrounding Mexico City and Johannesburg. Addressing antimicrobial resistance requires global, coordinated, multilateral efforts grounded in a One Health approach to reduce the misuse of antimicrobials. Part of this push will involve supporting research to better understand how our food systems contribute to and are affected by AMR and to develop alternatives that will work for food producers across the globe.
The way forward
Crises like COVID-19 expose the vulnerabilities in the food and health systems of many countries. Most often, it is resource-poor people living in difficult environments, including environments that are highly impacted by climate change, who are on the front lines. Investing in research for climate-resilient food systems can enhance global health, livelihoods and food security today and for future generations. The One Health framework can significantly contribute to advancing research and innovation towards this goal. Reciprocally, bringing a stronger dose of food systems expertise into One Health research will provide valuable insights when addressing the threat of AMR and zoonotic disease epidemics arising in food systems. COVID-19 has jolted us all to think more about resilience – our own, that of our health systems and that of our food systems. Linking these two powerful concepts and fields of research, we can act to turn the negative SDG trends around and build practical, more resilient, healthy, nutritious and sustainable food systems that work for everyone.
Tackling Rift Valley Fever Epidemics in Food Systems
In 2018, the World Health Organization named Rift Valley Fever (RVF) one of the world’s eight most threatening pathogens. This viral disease is endemic in Eastern Africa and the Horn of Africa region and affects goats, sheep, cattle and humans. Its outbreaks occur in irregular 5 to 15 years cycles. This disease poses a significant risk to human health and threatens the economic and food security of smallholder farmers in these regions. Although there is a vaccine against RVF, its uptake among smallholder farmers is limited because it is expensive and the incentive to vaccinate livestock during the long periods between outbreaks is low. Tackling this zoonotic threat requires working closely with smallholder farmers to develop solutions that consider the obstacles to vaccine uptake.
This is one of the diseases targeted by the Livestock Vaccine Innovation Fund (LVIF), a 57 million Canadian Dollar initiative supported by the Bill & Melinda Gates Foundation, Global Affairs Canada and the International Development Research Centre (IDRC) for the development, production and commercialisation of vaccines against neglected livestock and zoonotic diseases in sub-Saharan Africa and South and Southeast Asia. One of the LVIF projects is working to combine the RVF vaccine with other livestock vaccines that farmers routinely use to reduce these barriers to uptake.
Dominique Charron is Vice-President, Programs and Partnerships at Canada’s International Development Research Centre (IDRC). She holds a PhD in epidemiology and a Doctor of Veterinary Medicine from the University of Guelph, Ontario, Canada.
Evelyn Baraké is a Program Officer working in knowledge translation at Canada’s International Development Research Centre (IDRC).
Contact: ebarake@idrc.ca
References and further reading:
IDRC: Livestock Vaccine Innovation Fund
https://www.idrc.ca/en/initiative/livestock-vaccine-innovation-fund
IDRC: Development of 2 multivalent RVF vaccines for improved uptake in cattle and in small ruminants
Science: Global trends in antimicrobial resistance in animals in low- and middle-income countries
https://www.idrc.ca/en/research-in-action/development-2-multivalent-rvf-vaccines-improved-uptake-cattle-and-small-ruminants





Add a comment
Be the First to Comment