Download this article in magazine layout
Download this article in magazine layout
- Share this article
- Subscribe to our newsletter
One Health and wildlife trade(-offs) – preventing future pandemics
The COVID-19 pandemic is a painful wake-up call reminding us of factors that promote disease emergence and highlighting the critical control points at which we can reduce the risk for future pandemics: human activities expanding contact with wildlife and their habitats, such as farming, logging, housing and infrastructure development, capture for trade, and hunting, all of which increase the potential for viruses to spill over into human populations. The next pandemic could emerge at any time and might be even worse than what we are experiencing now. It is up to us to change the odds in our favour.
Pandemic origins, trends and risks
The COVID-19 pandemic has had an unprecedented and catastrophic impact on global populations with tragic illness and suffering, loss of lives, and devastating consequences for the global economy and livelihoods, many of which will reach far into the future. COVID-19 is a zoonotic disease with a wildlife origin. The majority of new infectious diseases that have emerged in humans since the 1940s are zoonotic, and 72 per cent of these diseases have come from wildlife, including Ebola virus disease, HIV/AIDS, and the severe acute respiratory syndrome, SARS. The frequency at which these novel diseases are emerging is increasing over time and so is the proportion of those which originate in wildlife. Scientists estimate that there are around 1.7 million viruses which have not yet been discovered in mammals and birds, of which about 700,000 may have the potential to jump to humans.
However, wild animals per se do not increase disease risk. It is the human activities that expand contact with wild habitats, including human encroachment into natural areas for hunting and capture of wildlife (especially for trade), land clearing for agriculture, infrastructure development and other causes of deforestation, forest degradation (e.g. through logging), and fragmentation that open new pathways along which disease can travel. Attempting to remove zoonotic threats by removing wildlife populations does not address the root cause, and may even have negative consequences that actually increase the risk of disease transmission by removing natural buffers within the intact ecosystem. So what can be done?
Drivers of risk: compromised ecosystems, wildlife trade and supply chains
Maintaining distance between human and animal activity – physical distancing – reduces the likelihood and thereby the risk that a virus or other pathogen can ‘jump’ from one host to another. To reduce the risk of future pandemics, we need to evaluate and reduce or eliminate detrimental overlap between humans, their livestock and wildlife. Since ecological degradation increases the overall risk of zoonotic disease outbreaks originating from wildlife, one important strategy is to reduce human encroachment by protecting highly intact ecosystems. Another one pertains to commercial wildlife markets for human consumption (food and medicine) and associated trade.
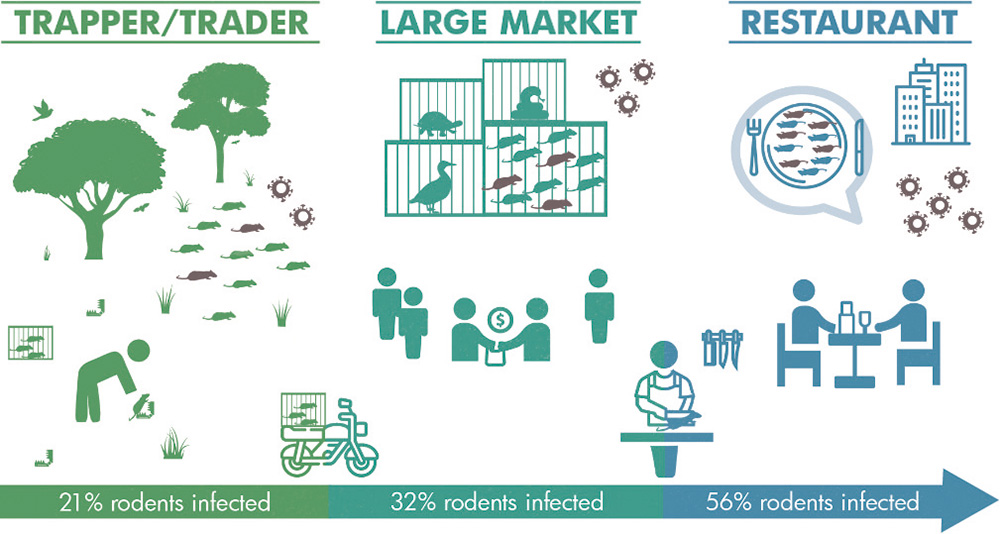
The pandemic risk of commercial wildlife markets was already recognised during the 2002-2003 SARS outbreak. Unfortunately, policy-makers failed to let this insight guide necessary changes. While almost all human coronaviruses are believed to have zoonotic origins or otherwise circulate in animals, wildlife trade is suspected to have created the conditions necessary for the SARS Coronavirus 1 and 2 (the latter causing COVID-19) spill-over and emergence in humans. The wildlife supply chain (including illegal and legal, sustainable and unsustainable, wild-caught and captive bred sources) involves conditions conducive to the emergence of zoonotic pathogens with pandemic potential. Stress in the animals (such as from cramped conditions, transport methods, mixing with other animals, etc.) increases expulsion and release of viruses and other pathogens, while the mixing of varied species of wildlife with domestic animals and slaughtering and butchering of fresh carcasses in crowded urban markets creates an optimal environment for viruses to exchange genetic material, pathogen transmission and spread. Furthermore, recent research suggests that, as wildlife moves along the wildlife supply chain, from capture sites to large markets, and on to restaurants, the likelihood of a positive coronavirus test result increases with each step from capture to consumption. Thus, each stage in the wildlife trade chain amplifies the chance of pathogen spill-over and novel viral emergence.
Considering the high numbers of everyday human-wildlife contact, spill-over events where a pathogen, such as a virus, jumps from a non-human animal species to a human are relatively rare (although the vast majority go unnoticed and are therefore underreported). Nonetheless, it’s a numbers game: the more opportunities created, the higher the chance of a spill-over occurring. This is exemplified by the increasing frequency of emerging infectious diseases stemming from wildlife, which reflects ever-growing contact points between human activity and wildlife habitat. And we now see that even a rare event, such as the virus causing COVID-19 or HIV/AIDS, can cause massive death, suffering, and devastation. While recognising that these events are rare, this must not preclude action. This increasing trend of spill-over events must be halted and reversed. We must work to lower the probability of these spill-over events as far as possible.
Context matters
There are stark geographic and context-specific differences when it comes to the pandemic risks and opportunities for mitigation. Evidence suggests that when there is a greater diversity of animal host species, the variety of virus types increases proportionately. This is one reason for areas with high biodiversity, such as those in forested tropical regions experiencing land-use changes, to have a higher risk of zoonotic disease emergence.
In countries with high species diversity, wildlife is often traded for meat, jewellery, curios, other products, traditional and non-traditional medicines, pets, or entertainment; for many countries, this trade is both domestic and international. There are, of course, regional differences. In some Asian countries, like China and Vietnam, where wildlife for food is predominantly a luxury item, governments are already moving to enact and implement important legislation and regulations to ban trade and consumption of wildlife (and China has already implemented laudable targeted regulations). In contrast, in Central Africa, for example, consuming bushmeat is a social norm, and there are large numbers of local people whose food security and livelihoods depend on wild meat consumption. But the majority of people in cities in Central Africa choose to consume bushmeat as a luxury item that is more expensive and does not relate to food security.
This high demand for luxury bushmeat in urban areas and wildlife trade encourages rural populations to hunt more animals than is necessary for their own consumption, thereby putting these communities at an added risk of zoonotic disease transmission and depleting resources for Indigenous Peoples and local communities (IPLCs) who rely on wild meat to meet their nutritional requirements. Policy change must be accompanied by a sustained and targeted effort to alter deep-rooted consumption practices and secure public support while respecting the rights and needs of IPLCs. This will, on a country by country basis, require certain adjustments to support existing cultural practices, formulate policy and enact appropriate legislation.
It is particularly important to ensure that private sector logging, mining, and plantation companies do not use the market closures to abrogate the legitimate rights of IPLCs who still depend on wildlife as a vital source of food, income and cultural identity, and whose effective, multi-generational stewardship has maintained most of the planet’s remaining ecologically intact ecosystems. Nevertheless, recognising and ensuring the needs and rights of IPLCs should never be used as a smokescreen to facilitate continuation of commercial trade and markets that pose an unacceptable pandemic risk on a global scale. Action, albeit in a domestic context, must be taken everywhere to reduce the chance of another zoonotic pandemic.
A One Health approach to mitigate epidemic/ pandemic risks
An integrated One Health approach, which fully acknowledges the interconnectedness and interdependence of human, animal, plant, and environmental health, as outlined in the “Berlin Principles on One Health”, adopted in 2019, is paramount in tackling some of the most pressing global health challenges, including the potential for future pandemics. The Berlin Principles update the “Manhattan Principles” from 2004, in which the term One Health was first coined for a broader public. These principles are an urgent Call to Action for cooperative, multilateral and engaged democratic efforts at all levels of society, in every country, and at international level.
By fully acknowledging the interconnectedness and interdependence of human, animal and ecosystem health, we can identify and implement pertinent and long overdue measures to reduce the risk of future pandemics (see boxed text). Additionally, many of the measures with this aim simultaneously help to mitigate some of the other major public health challenges of our time posed by the climate and biodiversity crises, which presents us with the rare opportunity to be in a triple-win position.
Recent analyses suggest that the cost of preventing further pandemics over the next decade by protecting wildlife and ecosystems would equate to just two per cent of the estimated financial damage caused thus far by COVID-19. The profits – legal and illegal – that are generated from the commercial trade in wildlife are negligible in comparison to the tens of trillions of dollars of economic devastation that we are now witnessing, and are even more negligible when limited to wildlife trade and markets for human consumption.
Currently expedited production of drugs and vaccines in response to the COVID-19 pandemic is a point of pride for some governments. If we are lucky and one of these products actually does prove efficacious and safe, and can be rapidly produced at scale, it will still have taken over a year to reach people with millions of deaths and terrible suffering in the interim. Large parts of the global health community are now calling for improved pandemic preparedness, e.g. through global collaboration initiatives, such as the ACT (Access to COVID-19 Tools) Accelerator, to escalate development, production and equitable access to pandemic disease tests, treatments and vaccines.
Of course, pandemic preparedness and response are very important. However, there are many challenges, some of which relate to the limitations and uncertainties of developing drugs and vaccines themselves. For some diseases, it took decades, while for others, vaccines and cures have yet to be found. Other hurdles include political challenges, e.g. the 2018-19 Ebola epidemic in Kivu, in the Democratic Republic of the Congo, became the second-largest Ebola outbreak in recorded history despite advanced containment measures, including widespread distribution of an effective vaccine, due to political instability within the affected region.
Moreover, drugs and vaccines cannot protect people from the spread of misinformation that undermines compliance with public health recommendations. Furthermore, not all epidemics and pandemics come in the immediately tangible form of a respiratory disease or haemorrhagic fever. The HIV/AIDS pandemic went unnoticed for decades, and it took further decades before an effective treatment could be developed. To this day, there is no vaccine against HIV, and according to UNAIDS, approximately 75.7 million people have become infected with HIV, 32.7 million of whom have died from AIDS-related illnesses since the start of the epidemic.
Therefore, we must not allow preparedness measures to create a false sense of security. Rather, prevention of disease emergence must be paramount. The human and financial costs associated with global pandemics will always be significantly greater than the price of measures to prevent them in the first place. Effective prevention is our greatest form of protection.
How to decrease the risk of zoonotic disease transmission
Preventing future pandemics requires a concerted effort to reconsider our interactions with our environment and to take important measures to reduce spill-over risks. The Wildlife Conservation Society supports a multipronged One Health strategy to lower the risk of zoonotic disease transmission, which should include:
1) preventing the degradation of ecosystems to preserve ecological integrity;
2) ending rural-urban supply and urban sale of bird and mammal species as wild meat;
3) ending urban demand for bushmeat;
4) reducing the risk of wildlife-to-hunter disease transmission in rural areas;
5) expanding early warning systems for emerging zoonotic diseases at the human, wildlife and forest (/habitat) interface; and
6) improving preparedness through strengthening public health infrastructure and outreach to protect the health of Indigenous Peoples and local communities.
Kim Grützmacher is currently Program Manager in the Health Program of the Wildlife Conservation Society (WCS). She is a veterinarian and holds a PhD in Biomedical Sciences which she obtained through her research in Germany’s Robert Koch Institute’s former junior research group “emerging zoonoses”.
Dr Chris Walzer is Executive Director of Health at the Wildlife Conservation Society. He is a board-certified wildlife veterinarian and professor of Conservation Medicine at the University of Veterinary Medicine in Vienna, Austria.
Dr Susan Lieberman is currently Vice President, International Policy with the Wildlife Conservation Society. She holds a PhD in tropical ecology from the University of Southern California, and has worked at the interface of conservation science and intergovernmental policy for more than 30 years.
Dr Amanda Fine is the Associate Director of Health at the Wildlife Conservation Society and oversees WCS health initiatives in Asia. She is a veterinarian with a PhD in epidemiology and has over 20 years of experience working at the intersection of wildlife, human and livestock health.
Contact: kgruetzmacher@wcs.org
References and further reading:
Quynh Huong, Nguyen et al.: Coronavirus testing indicates transmission risk increases along wildlife supply chains for human consumption in Viet Nam, 2013-2014. In: Plos One.
doi: 10.1371/journal.pone.0237129
WCS Website: Updates on COVID-19 Coronavirus
https://www.wcs.org/get-involved/updates/a-primer-on-the-coronavirus